Arteriovenous Malformation (AVM): Causes, Symptoms and Treatments
Fast facts:
An Arteriovenous Malformation (AVM) is a rare vascular anomaly consisting of tangled arteries and veins of varying sizes, which disrupts the normal blood flow and oxygen circulation in the brain.
A brain Arteriovenous Malformation may not show any symptoms until it ruptures, causing a haemorrhage. For some people, they might experience symptoms ranging from seizures to severe headache to loss of vision.
Treating an Arteriovenous Malformation largely depends on your age, health, size, and location of the anomaly.
What Is an Arteriovenous Malformation (AVM)?
Arteries and veins are blood vessels that carry blood around the body. Arteries are thick-walled tubes that carry oxygen-rich blood from the heart to the brain to keep it healthy. On the other hand, our veins are thin-walled tubes that conduct the now-oxygen-depleted blood to the heart to oxygenate it. An Arteriovenous Malformation disrupts this important process.
An Arteriovenous Malformation is a rare vascular anomaly consisting of tangled arteries and veins of varying sizes, which results in the disruption of the normal blood flow and oxygen circulation in the brain. It can occur anywhere in the body, but it mostly occurs in the brain, the brain stem, or the spinal cord.
Why arteriovenous malformations happen is still not clear. Doctors find that most people are born with AVM, but some are developed later in life. Approximately 3 of every 10,000 people are diagnosed with AVM, commonly occurring among men. They are rarely genetic.
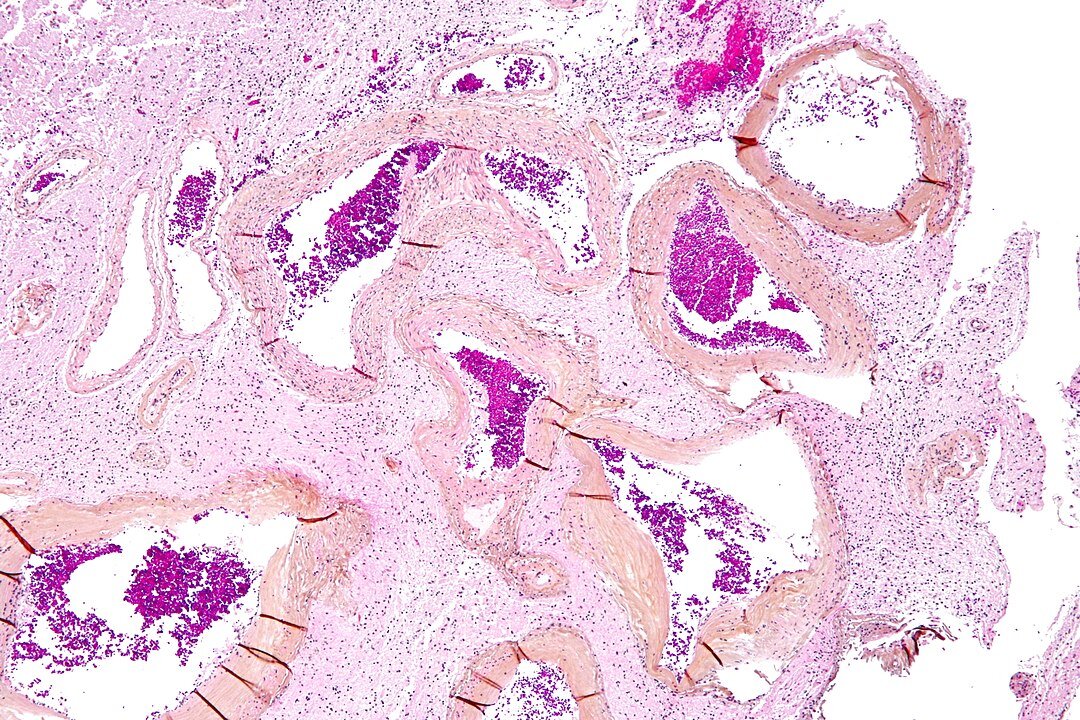
Low magnification micrograph of an arteriovenous malformation in the brain.
Image credit: Nephron, CC BY-SA 3.0, via Wikimedia Commons
Symptoms of an Arteriovenous Malformation
A brain Arteriovenous Malformation may not show any symptoms until one of two scenarios occurs: It is discovered while being treated for another illness or it ruptures, which then results in a brain haemorrhage. About 50% of the AVM cases have haemorrhage as their first symptom.
A bleeding AVM is life-threatening and requires hospitalisation.
Seek immediate medical attention by dialling 000.
Symptoms may include:
Seizures – 20 to 25% of AVM patients have focal or generalized seizures.
Localised or general headache - This is due to an increased blood flow around an AVM
Muscle weakness, numbness in one side of the body
Paralysis
Loss of vision
Difficulty in speaking
Confusion
Severe unsteadiness
Decreased sensation in any part of the body
Sleepiness, lethargy, disorientation, irritability
Stiff neck
Symptoms can worsen for some pregnant women because of changes in blood volume and blood pressure.
Symptoms become evident between the ages of 10 and 40 but are less likely to show when the patient reaches middle age.
Maximum-intensity projection from a CT cerebral angiogram showing an aneurysmal deep venous structure which drains to the vein of Galen, and then to an abnormal falcine sinus.
Image credit:Dr Laughlin Dawes, CC BY 3.0 via Wikimedia Commons
Vein of Galen Defect
This is a severe type of brain Arteriovenous Malformation, and its symptoms emerge immediately after birth. Symptoms include:
Noticeably swollen veins on the scalp
Seizures
Failure to thrive
Congestive heart failure
Diagnosis of an Arteriovenous Malformation
Your doctor will ask you questions about the symptoms you are experiencing. You will then go through a physical examination and some imaging tests (CT scan, MRI, or angiogram) to diagnose your condition.
Treatment of an Arteriovenous Malformation
Treating an Arteriovenous Malformation largely depends on your age, health, size, and the location of the anomaly.
The goal of treatment is to prevent haemorrhage and further complications. This is done by stopping the bleeding, controlling seizures, and if possible, removing the AVM.
Medical therapy. This is recommended for asymptomatic patients and patients whose AVM is in an area of the brain that can’t be easily treated.
Endovascular treatment. This is a minimally invasive procedure where the interventional neurologist inserts a catheter into an artery in your leg and, with an X-ray imaging as a guide, threads it through the blood vessels and into your brain. Once it’s in the feeding artery, the doctor injects an embolising agent that seals it and reduces blood flow into the AVM.
Open brain surgery. This is recommended for patients whose AVMs have bled or it is located in an area of the brain that is easily reached. In this procedure, your neurosurgeon temporarily removes a portion of your skull to get to the AVM. The goal is to seal off the AVM using special clips and remove it from the surrounding brain tissue.
Radiosurgery. This is recommended for small AVMs that are tough to remove via conventional surgery and for patients whose AVMs have not bled. Incision is not necessary; instead, radiation beams are used, causing the diseased blood vessels to scar and clot off in one to three years post-treatment.
DISCLAIMER: The information provided is designed to support, not replace, the relationship that exists between a patient or site visitor and their existing healthcare professionals.
Verified by: Dr Stephen Winters
Dr Hugh Stephen Winters is a neurologist with four years of exhaustive training in interventional neuroradiology, which includes a year of Clinical and Procedural Fellowship in Interventional Neuroradiology at the Erlanger Medical Center in Tennessee.


